
Payers have to effectively manage a tangle of ever-changing relationships between providers, groups, and member communities — all while handling traditional operational challenges like claims processing.
Today, member expectations are changing.
Meeting these new demands requires payers to step up their member engagement programs. Payers need to evaluate the best step forward for their organization to understand and address the needs of members in a succinct, member-centric manner that drives member satisfaction, improved health outcomes, and improved associate satisfaction in a trusting environment.
At Silverline, we’ve seen first-hand how Salesforce can help payers do just that. Here’s how:
The healthcare member engagement journey begins with members and caregivers and their ability to contact the call center agent through their preferred method of communication, whether that is through a phone call, text message, email, or other communication vehicles. Taking a member-centric approach requires you to support members where they are, rather than the way things have always been done. Texting, for example, is an often under-utilized channel that the vast majority of members prefer for healthcare-related interactions.
This doesn’t mean abandoning historical methods of communication but enhancing capabilities through a true “omni-channel” experience.
Building an omni-channel experience starts with workflow. Depending on the type of interaction, inquiries will be automatically assigned to queues to be worked by the agent most skilled at addressing the need, such as a multilingual agent speaking with a member in their native language. Data integrations with your existing systems create a single pane of glass for call center agents to verify a member’s identity (required by HIPAA), view demographic and enrollment information, and access previous member interactions through their health cloud console.
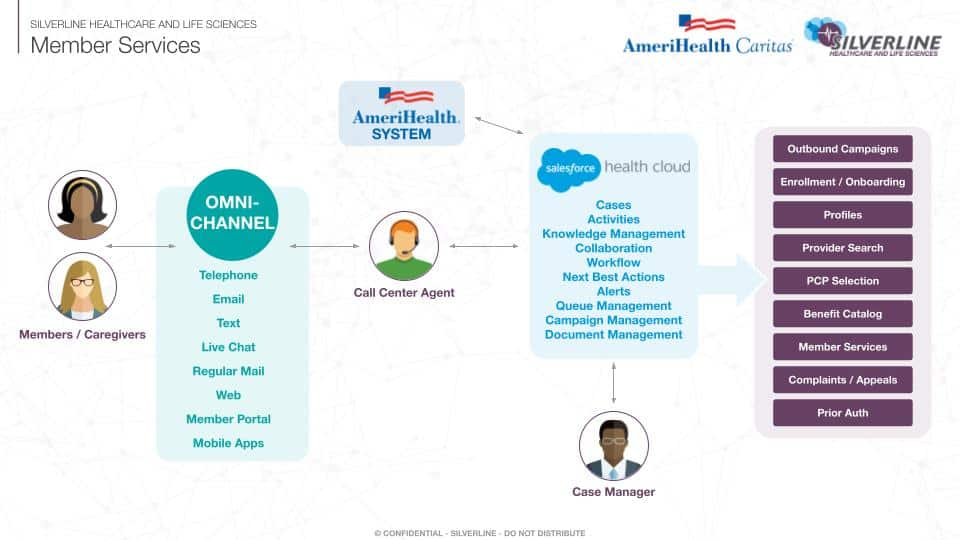
Using Salesforce’s Health Cloud tool, the Silverline team automates multiple touchpoints in the member services process, making it easier for your call center employees to provide a better experience — and your members to access the information they need, faster.
This includes:
By definition, when a patient engages with your team, they’re probably not at their best. Maybe they’ve just had a major surgery or a scary diagnosis. They could be facing months or years of chronic care management or a lifetime of managing a hereditary disease.
The member services journey isn’t just about one interaction with a call center agent. The journey stretches across the entire healthcare ecosystem, every time they engage with you, whether they are healthy, sick, or a caregiver. Take an active role in member health by proactively answering questions and assisting members with their healthcare.
By including all of the key pieces of member information in one place — from communication preferences to HIPAA documentation, information captured through health assessments, enrollment status, Medicaid benefits, social determinants of health, and life events — you can assist them with their healthcare journey.
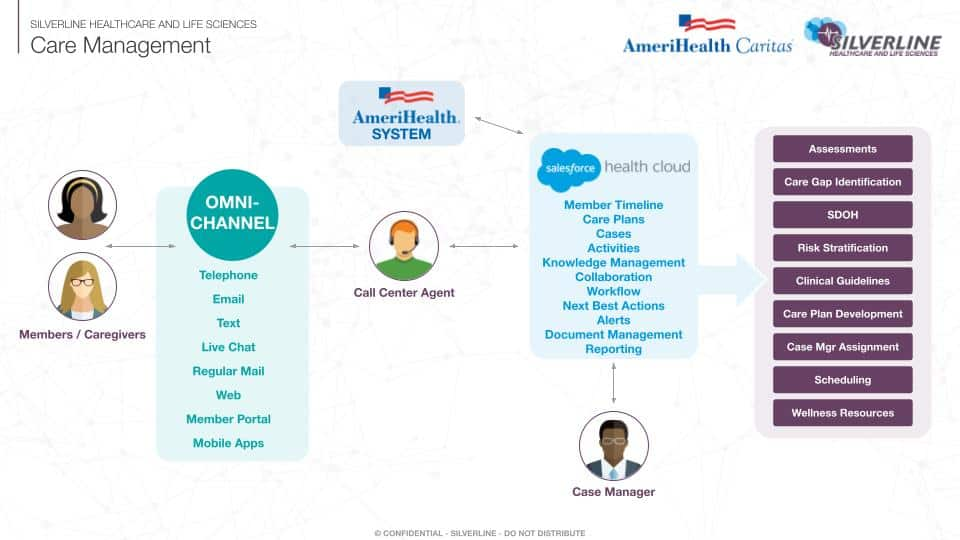
Using the Health Cloud platform, Silverline helps your care management team by:
At Silverline, we create long-term relationships with our clients by working with them on their strategic objectives, providing thought leadership, and ensuring the highest quality of services that suit their unique needs. We bring a holistic approach to a single source of truth for member services and other internal partners, improving first call resolution, decreasing wait time, and improving member satisfaction.
Whether you’re looking to attract, acquire, or administer new members, Silverline is here to help. Learn more about Salesforce for payers.
The original version of this page was published at: https://silverlinecrm.com/blog/healthcare/cracking-the-code-for-healthcare-member-engagement/
With real-world expertise in the Healthcare industry, including sub-segments such as Provider, Payer, Medical Device, and Life Sciences, Silverline helps clients realize continuous value on the Sal... Read more
Your members expect more of you than ever. They’re looking for a streamlined shopping experience, guidance when it comes to enrolling into the right plan, and that you’ll ...read more
As a payer, you know that your contractual relationships with different providers can be complicated. (Understatement of the year, right?)You’re dealing with different lines ...read more
At one time, providing high quality of care was enough to build a successful healthcare practice. Today, however, doctors and their staff must also provide high-quality, efficient ...read more
Contact centers are sometimes the afterthought of the healthcare provider ecosystem. They are often perceived as not offering much value and that the agents are just call takers that ...read more